Pre-order your autographed copy of Conversations About Brain Injury: Stories Shared at the Microphone.
Insights, Stories, and Resilience from a Decade of Podcast Interviews
An Introduction:
In the course of life’s unpredictable journey, there are moments that reshape us, molding our very existence into something new, uncharted, and challenging. A brain injury is one such moment—a profound, life-altering experience that can leave individuals and their loved ones grappling with uncertainty, resilience, and the quest for understanding.
Conversations About Brain Injury is a testament to the strength of the human spirit and the power of dialogue. Over the past decade, I have embarked on a remarkable journey of discovery, healing, and transformation after my own brain injury. Through the medium of podcasting, I’ve had the privilege of connecting with hundreds of remarkable individuals—survivors, caregivers, experts, and advocates—who have generously shared their stories, insights, and expertise with me and our global audience.
This book is a compilation of a few of those conversations, a heartfelt and enlightening mosaic of experiences that offer solace, guidance, and inspiration to those who have faced brain injury, as well as those who seek to understand the complex web of challenges and triumphs that often accompany it. Each dialogue is a unique and powerful exploration of the multifaceted nature of brain injury, delving into the emotional rollercoaster, the physical hurdles, the evolving identities, and the profound hope that emerges from adversity.
Within these pages, you will find the wisdom of parents who have dedicated their lives to caring for their injured children, the resilience of athletes who refused to let their dreams be shattered, the insights of neurologists who push the boundaries of medical science, and the courage of veterans who have navigated the shadows of war. You will encounter stories of loss, recovery, setbacks, and breakthroughs—all told with unflinching honesty and unwavering determination.
Conversations About Brain Injury is more than just a collection of interviews; it is a testament to the enduring human spirit and our capacity to find meaning and purpose even in the face of the most daunting challenges. It is a source of knowledge, empathy, and hope for anyone whose life has been touched by brain injury, directly or indirectly.
As you embark on this journey through these conversations, may you find solace, inspiration, and a renewed sense of the resilience that resides within us all. Together, we will explore the depths of the human experience, the intricacies of brain injury, and the profound strength that can arise when we dare to share our stories.
PRE-ORDER
All books have FREE US shipping
(NOTE: international shipping is only available on the single pre-order book)
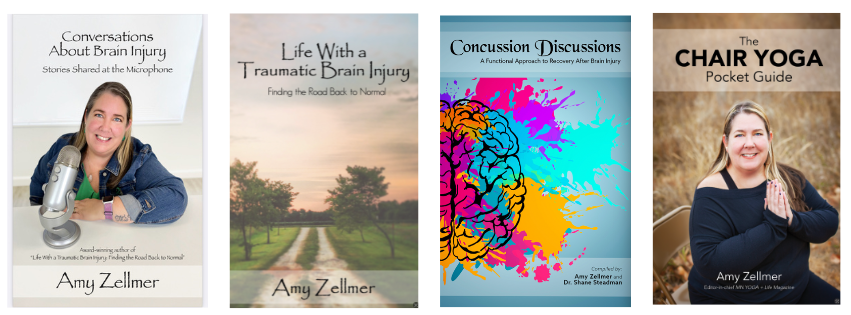
Pre-order an autographed copy of the book (free US shipping) $18**
Pre-order an autographed copy of the book (with international shipping) $40**
Pre-order a digital version of the book (PDF) and audio book file (MP4) (delivered via email) $50**
Conversations About Brain Injury PLUS Life With a Traumatic Brain Injury (US only) $35**
Conversations About Brain Injury PLUS Concussion Discussions (US only) $40**
Conversations About Brain Injury PLUS The Chair Yoga Pocket Guide (US only) $35**
Conversations About Brain Injury PLUS all three additional books (US only) $75**
FIVE copies of Conversations About Brain Injury (perfect for a book club) (US only) $90**
Orders will be shipped in early 2025
 Celebrity nutrition and fitness expert JJ Virgin’s life changed when her 16-year-old son Grant got hit by a car. Suffering a coma and severe injuries, the doctors believed Grant wouldn’t survive, but JJ refused to give up hope. She vowed to help him improve, and against all odds, Grant not only survived, but began to recover. JJ shares her insight on their journey towards improving her son’s health, and what life is like now.
Celebrity nutrition and fitness expert JJ Virgin’s life changed when her 16-year-old son Grant got hit by a car. Suffering a coma and severe injuries, the doctors believed Grant wouldn’t survive, but JJ refused to give up hope. She vowed to help him improve, and against all odds, Grant not only survived, but began to recover. JJ shares her insight on their journey towards improving her son’s health, and what life is like now. Thank you to our amazing presenters as well as the cast and crew from
Thank you to our amazing presenters as well as the cast and crew from 




 I was recently interviewed by
I was recently interviewed by